I Will Always Love You: The Importance of Advance Directives
Bobbi Kristina Brown's fight for life on a ventilator adds to the list of stories highlighting the need for all adults to execute advance directives.
The world was shocked when superstar singer and actress Whitney Houston was found unresponsive in a bathtub full of water on February 11, 2012. Perhaps even more shocking was when Houston’s only child, Bobbi Kristina Brown, was found in the same position nearly three years after her mother’s death, on January 31, 2015.
Though Houston was pronounced dead as soon as medical personnel arrived on the scene, her daughter has fought for her life in a Georgia hospital for over two weeks. Rumors have swirled about the twenty-one-year-old’s condition, including reports that she had been placed in a medically-induced coma and that she could only breathe with the help of a ventilator. Bobbi Kristina has been surrounded by family members throughout the ordeal, including her father Bobby Brown, grandmother Cissy Houston, and numerous cousins, aunts, and uncles. Some media outlets had reported that the family agreed to remove Bobbi Kristina from life support on the anniversary of her mother’s death, but for now it appears that she is still receiving medical treatment as her family continues to pray for her recovery.
In its first case on the “right to die” in 1990, the Court held that while a right to refuse medical treatment does exist, an incompetent person is unable to exercise such a right.
The Houston-Brown clan is far from the first family to wrestle with the question of whether to remove a loved one from life support in the face of a grim diagnosis. The first case to cause a widespread debate about the “right to die” arose after twenty-one-year-old Karen Ann Quinlan slipped into a coma after a night of heavy drinking and drug use on April 14, 1975. After doctors ignored Joseph and Julia Quinlan’s requests to take their daughter off of a respirator and allow her to die a natural death, the Quinlans turned to the courts for help. The New Jersey Supreme Court ruled in a 1976 decision that since there was “no reasonable possibility” that Karen Ann would recover, her right to privacy outweighed the state’s interest in keeping her alive. The Quinlans removed Karen Ann from the respirator, but continued to provide her with artificial nutrition and hydration. Karen Ann Quinlan lived in a vegetative state for ten years, succumbing to pneumonia on June 11, 1985.
Lester and Joyce Cruzan famously had to travel all the way to the U.S. Supreme Court to fight the State of Missouri for the right to remove their daughter, Nancy, from life support after a devastating car accident in 1983 left her in an irreversible vegetative state at age twenty-five. In its first case on the right to die in 1990, the Court held that while a right to refuse medical treatment does exist, an incompetent person is unable to exercise such a right. The Court found that the state had the constitutional authority to require that before the treatment could be withdrawn, “clear and convincing evidence” had to be shown to demonstrate that Nancy would have refused the treatment.
After the Supreme Court ruling, the Cruzans were granted a second hearing before a probate judge at which they presented new evidence that Nancy would not have wanted to be kept alive by a feeding tube. The judge found that this new evidence met the state’s standard and granted their request to remove the feeding tube. Nancy Cruzan’s feeding tube was removed on December 14, 1990. She died twelve days later.
At the same time that the Cruzans were fighting their battle against the State of Missouri, the family of Theresa “Terri” Schiavo was fighting a similar battle amongst themselves. On February 25, 1990, twenty-six-year-old Terri collapsed in her Florida home. Though doctors could not determine what exactly caused the chemical imbalance that stopped Terri’s heart, they agreed that her brain had been deprived of oxygen long enough to leave her in an irreversible vegetative state. Like Nancy Cruzan, Terri was able to breathe on her own, but had to be fed through a feeding tube.
The fight between Terri’s husband, Michael Schiavo, and her parents, Robert and Mary Schindler, over the decision to remove Terri’s feeding tube caused a national debate. Michael believed that Terri would not want to be kept alive by a feeding tube, while the Schindlers held onto the hope that their daughter would recover. In a legal battle that lasted fifteen years, Florida state courts primarily sided with Michael, granting him the right to remove the feeding tube in 2001 (until another court ordered the tube reattached two days later) and again in 2003.
After the 2003 ruling, then-Governor Jeb Bush pushed “Terri’s Law” through the state legislature. The law granted Gov. Bush the authority to intervene in the case and feeding tube was again reattached. The Florida Supreme Court struck down the law as unconstitutional the following year, at which point federal lawmakers became involved. In March 2005, President George W. Bush (the governor’s brother) and Congress enacted a law which transferred jurisdiction over the case to the federal courts. Federal courts declined to overturn the state courts’ rulings, and Terri Schiavo died on March 31, 2005.
While patients in a persistent vegetative state will show some signs of low-level brain activity, even breathing on their own, patients with brain death have no brain activity at all.
The recent case of Marlise Muñoz had an extra layer of complication—she was fourteen-weeks pregnant when her husband, Erick Muñoz, found her unconscious on the kitchen floor in their Forth Worth home. Doctors discovered that thirty-three-year-old Marlise had developed in a blood clot in her lungs and declared her brain dead two days after she arrived at John Peter Smith (“JPS”) Hospital on November 26, 2013.
While patients in a persistent vegetative state will show some signs of low-level brain activity, even breathing on their own, patients with brain death have no brain activity at all. Brain death is the standard for legal death, but brain dead patients can be kept on life support under certain circumstances. Officials at JPS Hospital argued that Texas Health and Safety Code § 166.049, which bars “withdraw[ing] or withhold[ing] life-sustaining treatment […] from a pregnant patient,” prevented them from removing Marlise from life support.
Erick filed a lawsuit against JPS Hospital, arguing that § 166.049 did not apply to Marlise because she was already dead. Instead, the lawsuit alleged that the law was unconstitutional because it violated Marlise’s right to privacy. The Muñozes were paramedics and had talked about how they would not want to be kept on life support in such a situation. The hospital argued that the law was designed to give the fetus a chance at life, therefore the state’s interest in protecting the fetus outweighed Marlise’s wishes. However, the fetus was not viable at the time Marlise was admitted to the hospital, and by the time of the lawsuit it had developed severe deformities in its brain, heart, and lower extremities. On January 24, 2014, a judge ordered that Marlise be taken off of life support. After deciding to forego an appeal, the hospital complied on January 26, 2014.
The best way to ease the pain of an already grieving family and to ensure that your wishes are carried out is to execute an advanced directive.
Though most of the women in these cases had discussed their feelings about life support with loved ones, their sad stories show that merely talking about our desires in such a situation is rarely enough. The best way to ease the pain of an already grieving family and to ensure that your wishes are carried out is to execute an advance directive. There are three types of advance directives available: power of attorney/healthcare power of attorney, living will, or do not resuscitate/do not intubate (“DNR/DNI”) orders.
Power of Attorney
Granting power of attorney allows another person, often called the “attorney in fact,” to make legal decisions for you. While healthcare decision making powers can be granted as part of a standard power of attorney, a specialized healthcare power of attorney is also available. The healthcare agent appointed by a healthcare power of attorney can make healthcare decisions for the subject of the power only after that person becomes incompetent to make healthcare decisions.
The power given to the healthcare agent may be limited, for example the subject of the power may specify whether artificial hydration or nutrition should be given and what types of mental health treatments are authorized. The subject of the power may also give the agent directions regarding organ donation and funeral arrangements.
Living Will
A living will allows you to specify which medical treatments you would or would not want in the event of incapacity. The standard living will in North Carolina, also called an “Advance Directive for a Natural Death,” contains directions concerning artificial hydration and nutrition and other “life-prolonging measures.” A living will may be used on its own or in conjunction with a healthcare power of attorney.
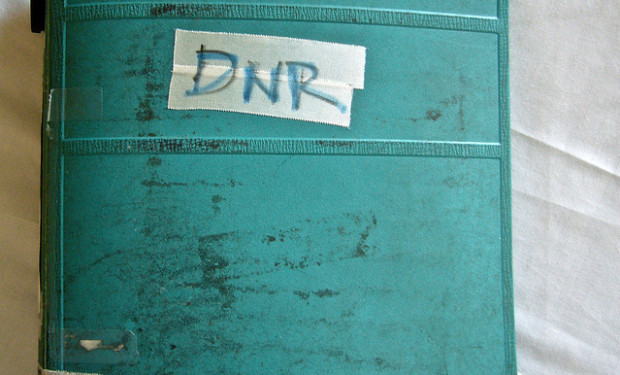
DNR/DNI Order
When a patient has a DNR order in place, this signifies that the patient does not want cardiopulmonary resuscitation performed in the event of cardiac or pulmonary arrest. A DNI order means that the patient does not want to be intubated, or have a plastic tube inserted in order to keep the airway open and ease breathing. DNR and DNI orders are often used in combination. In North Carolina, a MOST (Medical Orders for Scope of Treatment) is also available. Like a DNR or DNI order, a MOST is also a direct order to doctors about the type of treatment a patient does or does not want, but a MOST allows the patient greater flexibility in outlining the desired treatment.
Advance directives cannot prevent or cure an injury or illness, but they may be a great source of comfort to family or friends already struggling with a loved one’s deteriorating condition. Many people, especially young people, put off executing advance directives because they believe they don’t need one, or at least not right now. The fact that the longest fights and biggest cases concerned advance directives have all involved healthy young people suggests that healthy young people may need advance directives in place more than they thought.